It was there, a dark crescent moon creeping across the corner of my right eye, but no one could see it.
Only I could see it.
That dark shadow had been there for several weeks. Better not wait a month for my regular eye exam, I decided. Better say something now.
Good thing I did. “You’re having surgery as soon as possible,” I was told.
Here's how that winter day unfolded.
Mid-morning, the 10 a.m. hour: I called BayCare Clinic Eye Specialists, where I’ve been going for more than 30 years. An ophthalmic triage assistant called back almost immediately. “You need to come in right away,” she says.
1:40 p.m.: Dr. Jeffrey L. Shere examines my eye. He specializes in retina and vitreous issues and is a fellowship-trained vitreoretinal surgeon. He doesn’t like what he sees.
There’s a detached retina in my right eye. There’s no pain, and it hasn’t affected my vision beyond the lingering shadow, but the retina is torn halfway across my eye.
Why the rush to surgery? We need to save the sight in my right eye.
(A detached retina occurs when the retina pulls away from the lining of the inner back wall of the eye, allowing vitreous fluid to seep inside or beneath the retina.)
10:30 p.m.: I’m at Aurora BayCare Medical Center in Green Bay, getting prepped for eye surgery. It’s scheduled for 12:30 a.m., but there are two surgeries ahead of mine, and I get bumped.
2 a.m. the next morning: Shere performs surgery to repair the detached retina in my right eye. In recovery, I’m asked to lay face down on a special pillow to keep the surgically repaired eye stable. Do that for as long as you can, the nurse says. That turns out to be two hours, and then I’m sent home.
9 a.m. the next morning: I’m back at BayCare Clinic Eye Specialists, where Dr. Wei-Chuan Wang examines my surgically repaired eye. He, like Shere, specializes in retina and vitreous issues and is a fellowship-trained vitreoretinal surgeon.
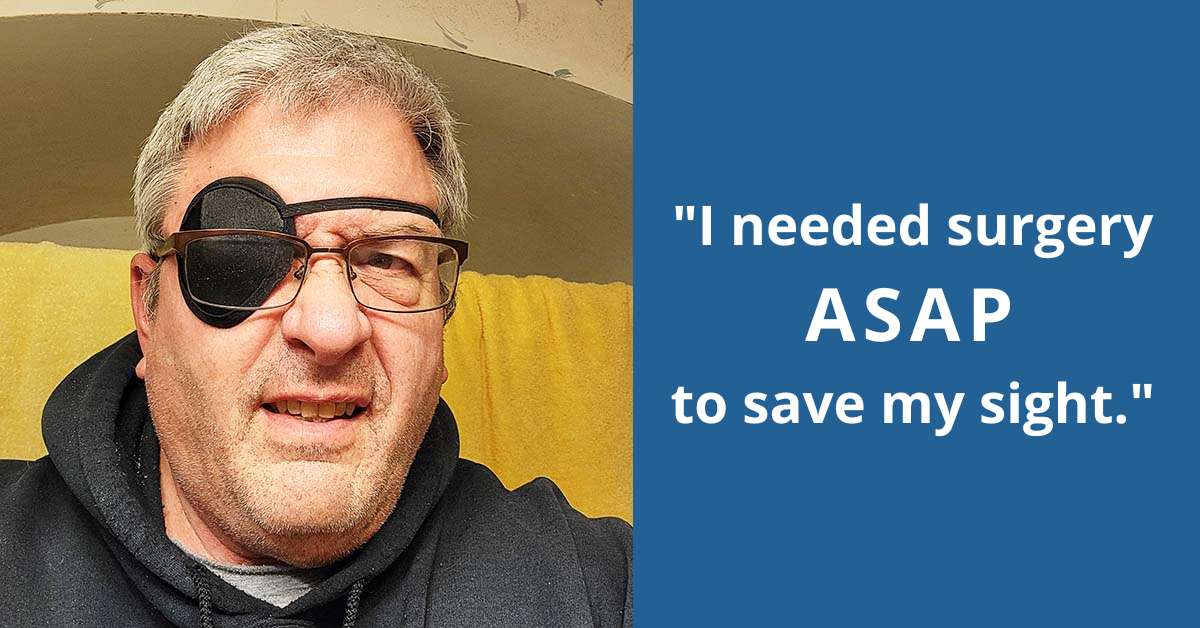
Everything looks good, Wang says. But no driving, no work, no activities for at least the next seven days as the eye heals. I’m wearing an eye patch with orders to keep my head up. I need the eye patch to see clearly. It covers the blurred vision in my right eye.
Part of the surgery involved putting a gas bubble into my right eye to hold the repaired retina in place for proper healing. Only I can see the gas bubble. It looks like the surface of a pond covering the lower half of my eye.
Ten days out from surgery, another follow-up visit: I have improved and mostly clear vision in the top of the eye, but the pond is still there, getting ever so slightly smaller each day. I’m still wearing the eye patch. Shere gives me the OK to return to activities.
13 days out from surgery, I resume driving. My vision is improved enough that I don’t need the eye patch to drive.
19 days out from surgery, the pond disappears. The gas bubble holding the repaired retina in place has dissipated. My vision is a little better every day. I’m not wearing the eye patch much anymore.
Final follow-up visit, almost eight weeks after surgery: Shere pronounces me good to go. Successful detached retina repair. My vision in the right eye is so good, he says, that it could be in the 20/15 to 20/20 range next time I get new eyewear.
That I had a detached retina really wasn’t a surprise. Those most at risk of having a detached retina are:
- Men
- People over 40
- Nearsighted people
- Those who have had cataract surgery, torn retinas or eye injuries
I check all those boxes. I’d been on a watch list for a detached retina for some time. I just didn’t know what to watch for.
Symptoms of a detached retina include flashes of light, increased eye floaters and darkening of peripheral vision.
That last thing – darkening of peripheral vision – was the dark crescent moon creeping across the corner of my right eye, the shadow only I could see.
Dr. Jeffrey L. Shere and Dr. Wei-Chuan Wang see people in Green Bay and Marinette. To request an appointment, call 920-327-7000 or 877-462-9465 in Green Bay or 715-732-4181 in Marinette, or do so online.